Haemorrhoid Surgery
Patient Information
What are Haemorrhoids?
Haemorrhoids are also called ‘piles’. They are the normal part of the lining of the inside of the anus. They are situated about 4 cm inside the bottom and act like cushions, containing blood vessels. Their function is to help with the control of evacuation of stool. This means that everyone has haemorrhoids. However, when patients describe that they have ‘haemorrhoids’ or ‘piles’, this is because they have symptoms related to them. Approximately one in two people in the general population will suffer with symptoms related to haemorrhoids.
What are the symptoms related to Haemorrhoids?
The commonest symptoms related to haemorrhoids include bleeding after or with a bowel motion, discomfort or pain around or inside the bottom, a mucus discharge, itching around or inside the bottom (called pruritus ani), or prolapse (when the haemorrhoids protrude from the bottom either permanently or only during a bowel motion.
Why do patients have these symptoms?
Haemorrhoids are cushions containing blood vessels. Anything that causes increased pressure within these cushions, or reduces the elasticity of the tissue which helps support them in position inside the anus, can lead to the haemorrhoids either enlarging or prolapsing. When they enlarge, they are more likely to bleed during a bowel motion and cause discomfort. Therefore, haemorrhoids are more common in pregnancy, in patients who chronically strain on the toilet or in the gym or at work and are also more common in the elderly.
What treatments are available for symptoms?
The important thing is to make a diagnosis of haemorrhoids. If you experience any bleeding from your bottom, the most likely diagnosis is haemorrhoids, but it is important to seek the advice from your doctor and even a colorectal specialist to rule out other causes of bleeding.
Increasing the fibre in your diet may soften the stools and lead to less discomfort and bleeding. Ointments, creams or suppositories may be prescribed. These usually include a low dose of local anaesthetic and steroid to soothe the area and reduce any inflammation. They are good at relieving symptoms which are mild and due to small haemorrhoids.
If haemorrhoidal symptoms persist, there are a number of minor treatments which are available when you see a colorectal specialist:
Injection sclerotherapy is a treatment which can be given during an outpatient consultation. A small probe is inserted into the bottom without anaesthetic to allow visualisation of the anus and lower part of the rectum. Approximately 5-10 mls of a sclerosant, 5% phenol in almond oil, is injected through the probe into the lining of the inside of the bottom. There is mild discomfort associated with this procedure, but this lasts usually only a few minutes but sometimes up to a few hours. This procedure may need to be repeated two to three times over a period of several months to allow this to be as effective as possible. The long term success of this treatment in relieving haemorrhoidal symptoms is 40%-50% and it is usually only recommended for patients with small haemorrhoids. The sclerosant acts by creating scarring, shrinking the haemorrhoids. Side effects of this treatment include bleeding and infection which are uncommon, but if they occur, you should contact your specialist or your local hospital immediately.
Infra-red photocoagulation is another treatment which can be given during the outpatient consultation. As with injection sclerotherapy, a probe is inserted into the patient’s bottom. The doctor uses a device that is inserted into the probe and creates an intense beam of infrared light. Heat created by the infrared light causes scar tissue, which again either shrinks the haemorrhoids or prevents them from bulging or prolapsing. The long term success of this treatment is 50%, but it is only reserved for patients with small haemorrhoids. The main side effects are discomfort following the procedure and bleeding which is uncommon.
Banding of haemorrhoids is a treatment which can either be given during the outpatient consultation or as a day case patient in a hospital. As with the other minor procedures, this is undertaken without anaesthetic. A small probe is inserted into the bottom to allow adequate visualisation of the haemorrhoids. A device is inserted though the probe containing small rubber bands approximately 0.5 cm in diameter. Three to four rubber bands are applied to the tissue immediately above the haemorrhoids. The bands cut off the blood supply to the tissue, which then shrinks and scars over a period of a few weeks. The scar tissue reduces the size of the haemorrhoids and makes them less likely to prolapse. The rubber bands usually drop off after 5-10 days following the procedure and pass either in the stools or are visible in the toilet after a bowel motion. The long term success of this procedure is 50%-60% in relieving haemorrhoidal symptoms. Side effects include discomfort which is quite common and usually settles after two to three days. Sometimes, if the bands are applied too low, the discomfort can be quite severe. If this occurs, you should contact your colorectal specialist or your local hospital immediately. Bleeding is quite common after the procedure and consists of a small amount of blood either in the toilet or when wiping with toilet paper. This usually settles. Very rarely, there can be a lot of bleeding. This can occur when the bands drop off leaving a raw area. If this occurs, please contact your colorectal specialist or your local hospital immediately.
What surgical procedures are available to treat haemorrhoids?
The oldest method of surgically treating haemorrhoids is by removing them under a general anaesthetic, a procedure called haemorrhoidectomy. This is very effective, approximately 95% success in relieving haemorrhoidal symptoms, but results in a long recovery period. Most patients have pain or discomfort for at least six weeks, with other associated symptoms including urgency (a feeling of having to rush to the toilet to pass a bowel motion), bleeding, risks of incontinence (weakness of the muscles of the bottom) and infection of the wounds. For these reasons, other procedures have evolved to treat haemorrhoids, without causing such a long period of pain and allowing the patient to return to normal activities much sooner.
Haemorrhoidal Artery Ligation and Rectoanal Repair (HALO)
This is the main surgical procedure that I perform for haemorrhoids and one that I would recommend for patients requiring haemorrhoidal surgery.
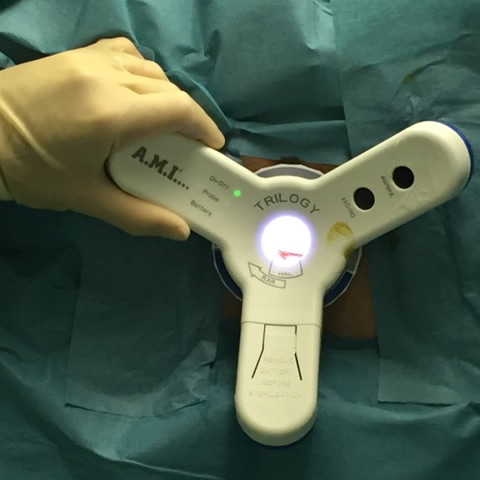
In 1995, a surgeon called Morinaga developed a surgical technique for the treatment of haemorrhoids which did not involve removing any tissue.
The current operation uses a miniature Doppler ultrasound device to locate all the arteries supplying the haemorrhoids as they come down from the rectum under the lining of the bowel. The device is inserted into the patient’s bottom during surgery. It has a small window which allows a stitch to be placed around the artery thus cutting off the blood supply to the pile. During the course of the procedure all the arteries supplying the piles are located and tied off (Ligation). After this ligation, I perform the ‘Rectoanal Repair’ which involves stitching the haemorrhoids back up to their original position in the anal canal. This is particularly useful for patients who have prolapsed haemorrhoids (where the haemorrhoids protrude from the bottom). Over several weeks, the haemorrhoids shrink and become fixed in a higher position inside the bottom. The stitches are absorbable and do not have to be removed.
The surgery is undertaken usually under general anaesthesia (asleep) but may also be undertaken under spinal anaesthesia (injection into the spine to make the bottom numb during surgery). The procedure lasts approximately 45 minutes and patients are usually well enough to be discharged from hospital on the same day.
What should I expect after surgery
Following surgery, patients are discharged the same say with painkillers and a laxative to avoid constipation. A small number of patients may experience difficulty in passing urine and this occurs particularly with men who have had pre-existing problems with passing urine. If this occurs, this usually settles after a few days.
The majority of patients do experience pain after this surgery. The pain usually lasts for one week, but some patients experience discomfort up to two weeks following this procedure. The degree of pain is variable, some patients describing very little pain at all, but some do have a lot of pain particularly in the first week which can be controlled with painkilling tablets.
A number of patients experience urgency, a feeling of having to rush to the toilet to open the bowels. This is due to irritation of the rectum by the stitches and usually settles after one week.
Bleeding is uncommon after this surgery, but the passage of a small amount of blood may be passed with a bowel motion in the first few days. This usually settles completely. If there is a large amount of bleeding, you should contact your colorectal specialist or local hospital immediately.
Infection is also uncommon after this procedure. This may be suspected if the rectal pain worsens after a few days and there is a discharge from your bottom with a bad odour. If this occurs, a course of antibiotic tablets should be prescribed.
The majority of patients should expect to be off work for one week following the HALO procedure.
What are the results of HALO surgery
This is a very successful procedure. 85% – 90% of patients describe almost complete resolution of their symptoms. The procedure is particularly successful at eliminating rectal bleeding. Prolapse is generally improved, but it is important to stress that this is not a cosmetic procedure and therefore anal skin tags (lumps from around the anus) may still persist after surgery. The discomfort caused by haemorrhoids is also improved to a great extent. There are a large number of patients who have undergone the HALO procedure who are so happy with the results that they have regretted not having this procedure years previously because of fear of haemorrhoid surgery.
Are all patients suitable for HALO surgery
Not all patients are suitable for HALO surgery. An assessment by a colorectal specialist in the outpatient clinic is necessary to make a decision about suitability.